Hospital Health Fund Fees – Same Day Fees Set Up
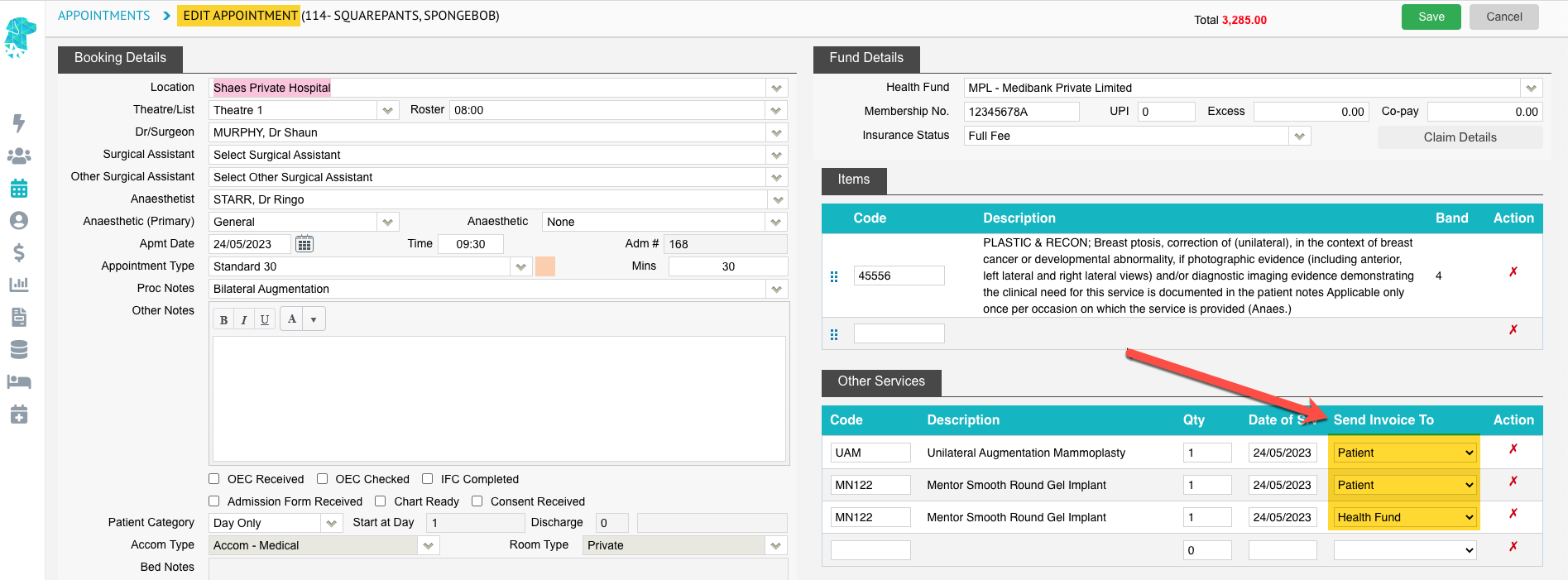
When new contracts are negotiated with health funds, amended fees need to be loaded into FYDO to facilitate a seamless IFC & Billing process.
- Fees can be entered in Settings > Hospital > Fees Setup
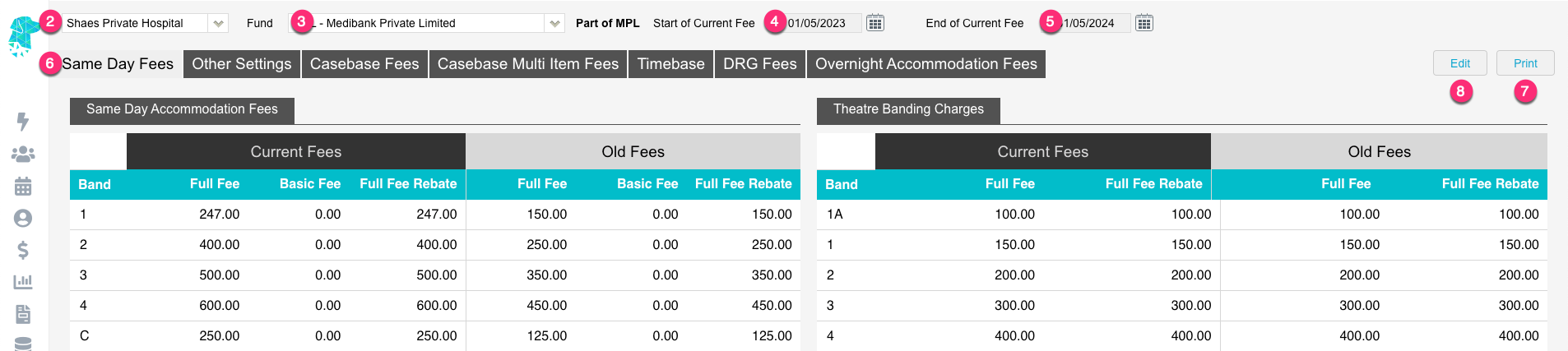
- For multi location databases, ensure the correct Location is selected
- Use the Fund drop down to select the required health fund
- The Start of Current Fee date indicates the date that the Current Fees will be utilised from. Any episode from before the start date will utilise the Old Fees
- The End of Current Fee date indicates the date that the Current Fees will expire. Users will still be able to create IFC’s for admissions after the End of Current Fee date. However, the system will prohibit billing for episodes that fall after this date. (This date isn’t mandatory. However, it is a good way to ensure accounts aren’t accidentally billed at outdated prices)
- The Same Day Fees tab contains the Same Day Accommodation Fees and the Theatre Banding Charges
- Users are also given the ability to Print the health fund fees, for the selected fund
- To edit these fees, click the Edit button
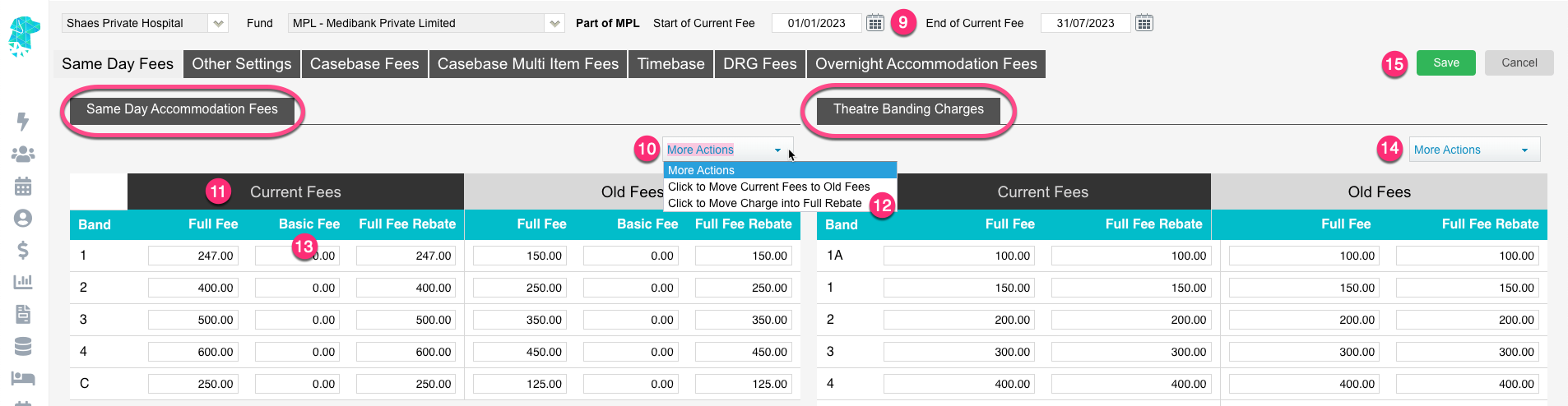
- Once in edit mode, you will be able to amend the Start of Current Fee & End of Current Fee dates to indicate when the new contract fees apply
- Use the More Actions drop down to Click to Move Current Fees to Old Fees before the new fees are entered. This will replicate all the current accommodation fees into the Old Fees columns
- Enter the new fees in the Full Fee column for the corresponding bands. (C is for Type C procedures)
- Once all Full Fees are entered, use the More Actions dropdown, and select Click to Move Charge into Full Rebate. This will copy all fees from the Full Fee column over into the Full Fee Rebate (Do not do this step for un-insured fees or for other ‘funds’ that don’t attract a rebate)
- Depending on the contract agreement, facilities may need to add the Full Fee amount into the Basic Fee column. This can easily be done by using the More Actions drop down.
- Repeat the same steps 10 > 12 for the Theatre Banding Charges on the right side of the screen
- Click Save
For further information on how to set up fees, please visit our pages:
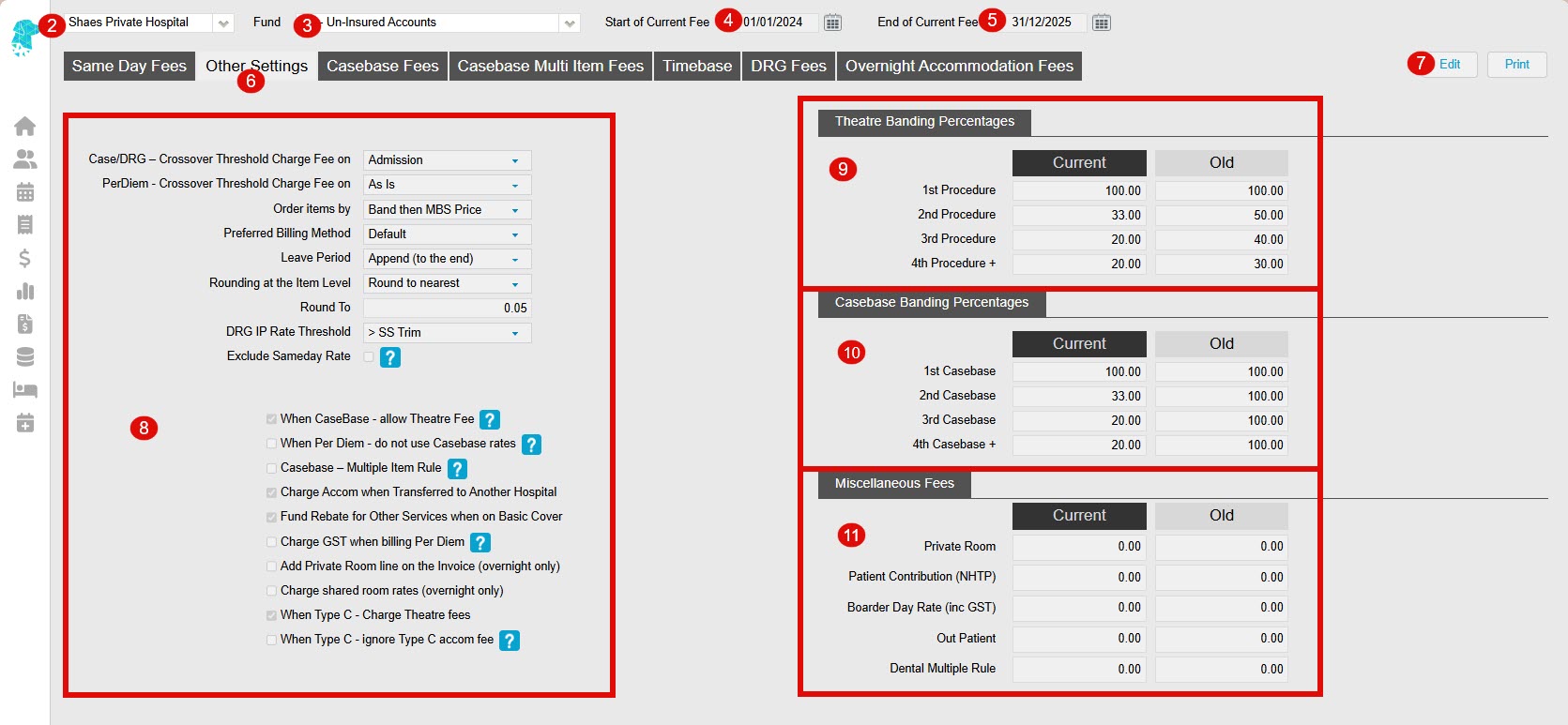
Other Settings
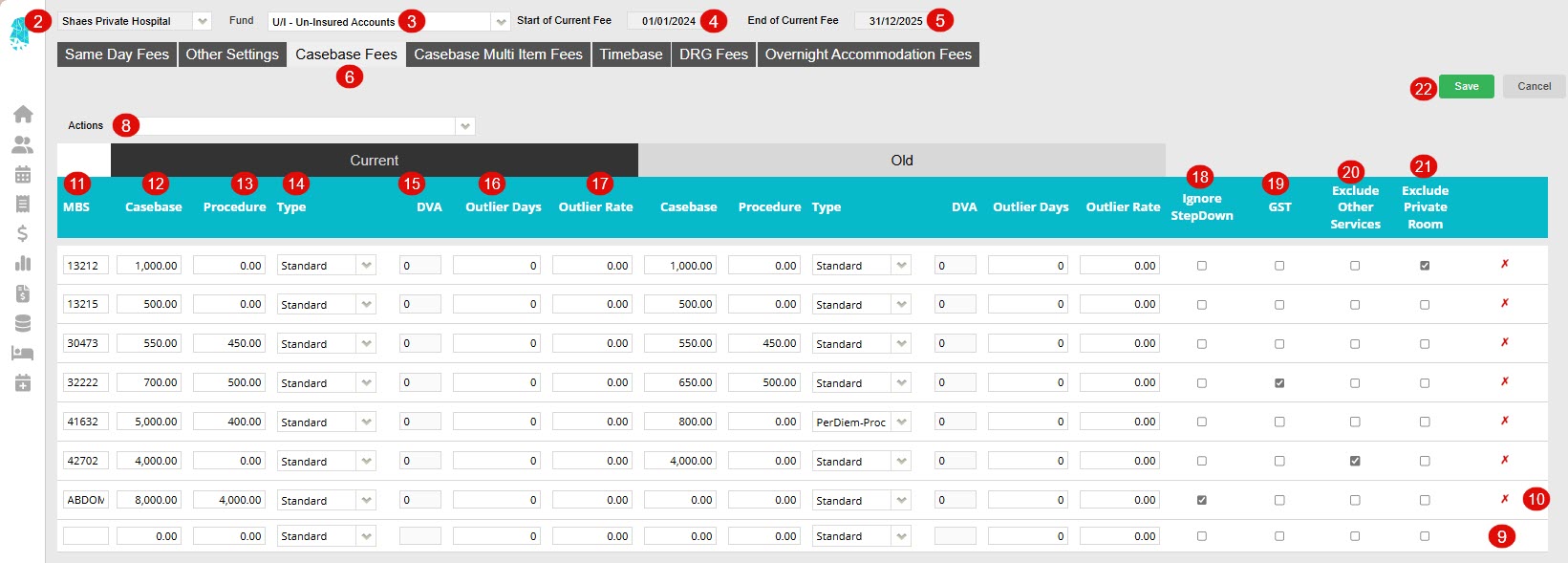
Casebase Fees
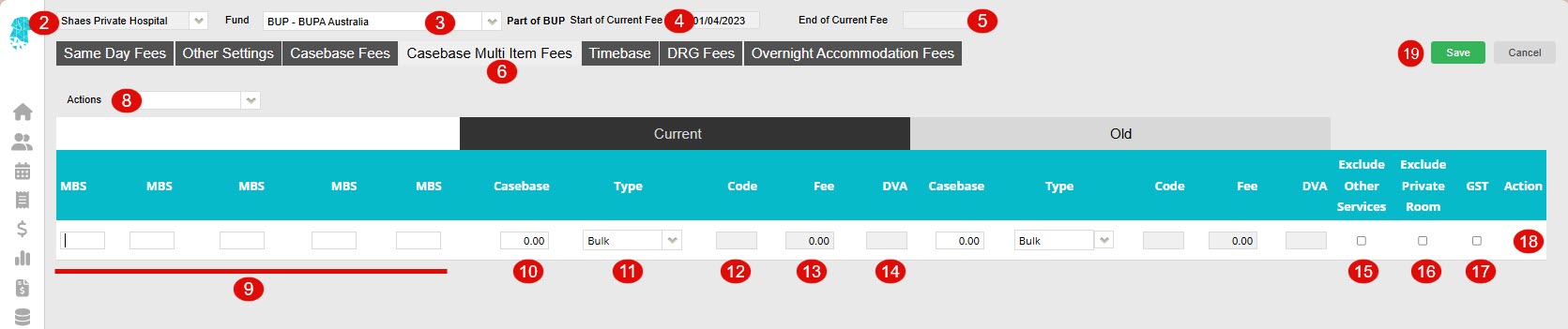
Casebase Multi Fees
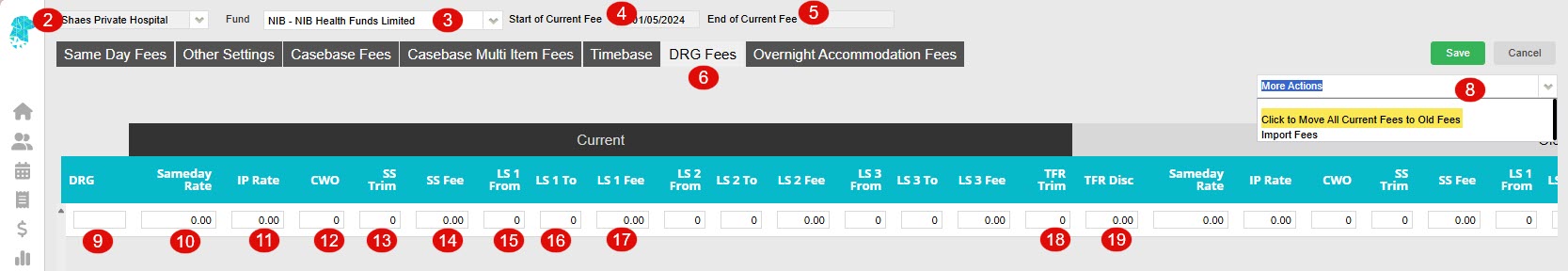
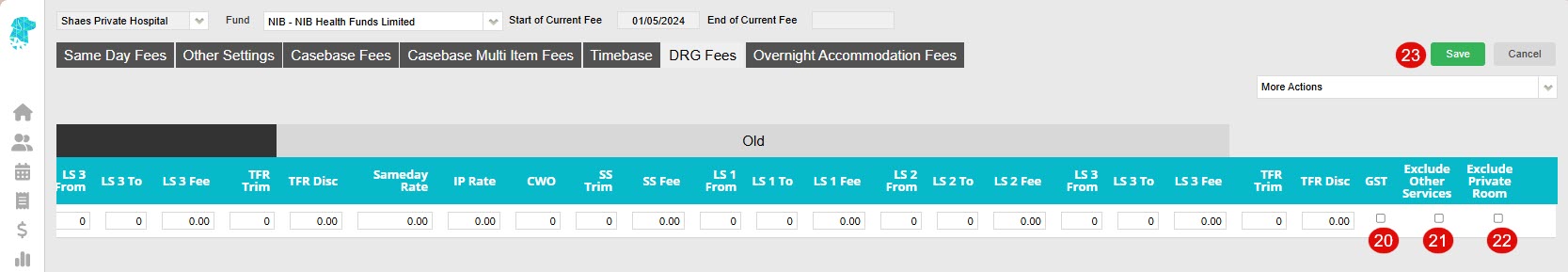
DRG Fees
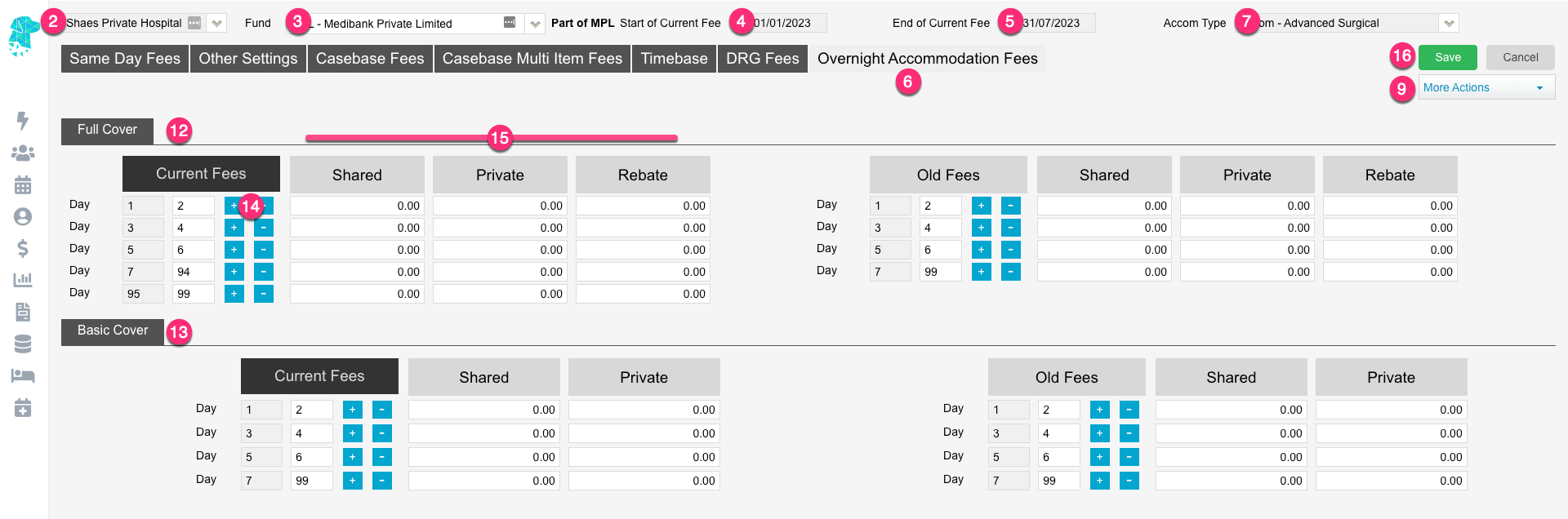
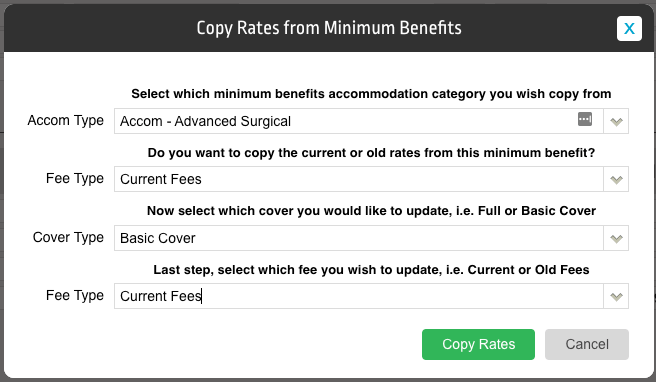
Overnight Accommodation Fees