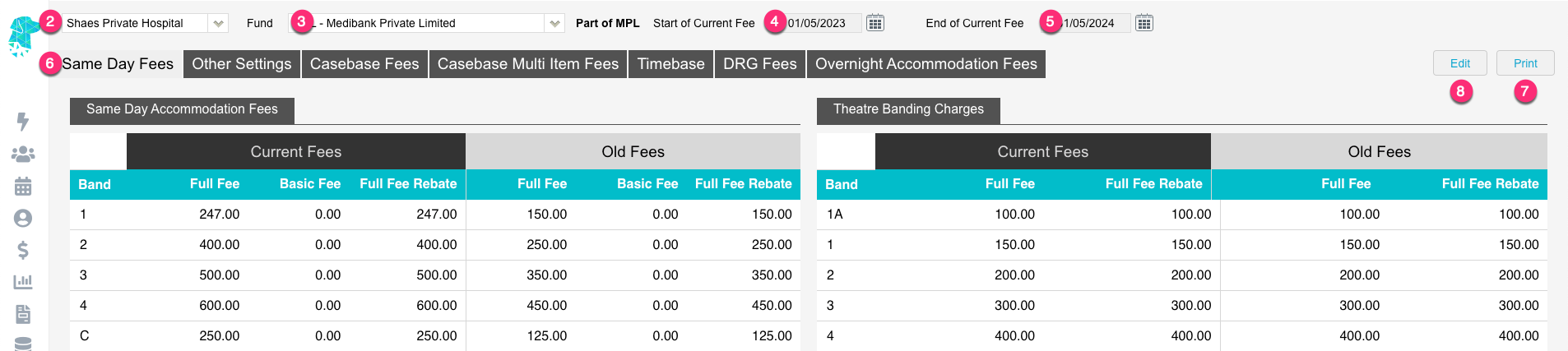
There will be some instances where insured patients need to pay for part of their procedure.
Maybe some of the procedures is classified as a cosmetic procedure, maybe they have restrictions on their level of cover & the hospital is able to raise a charge to the patient for those extra procedures.
Maybe the hospital is contracted for 2nd Tier rates and can charge a patient gap or they want to charge a credit card surcharge to the patient.
Whatever the case may be, FYDO accommodates this split method of billing the health fund AND the patient seamlessly.
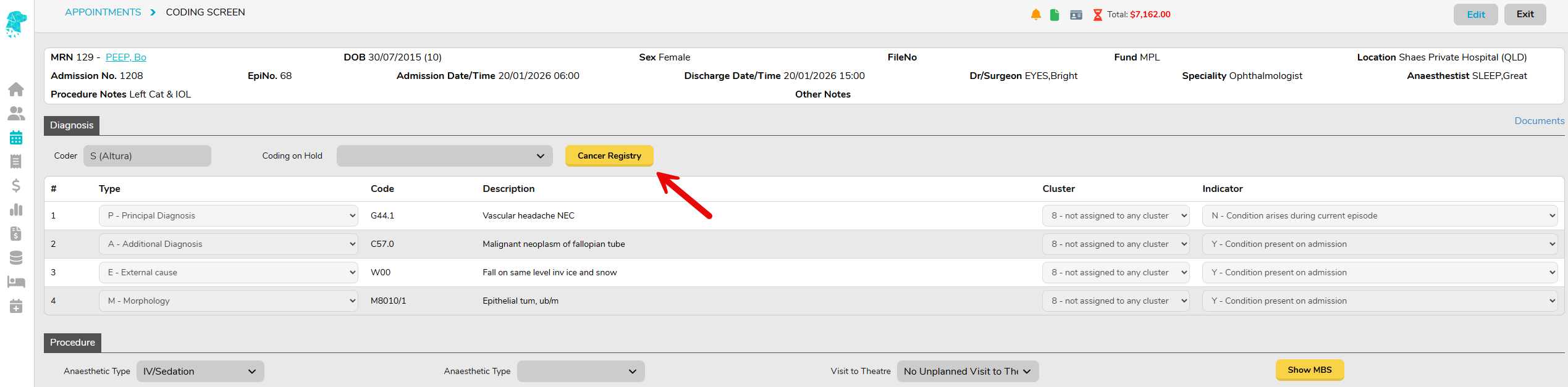
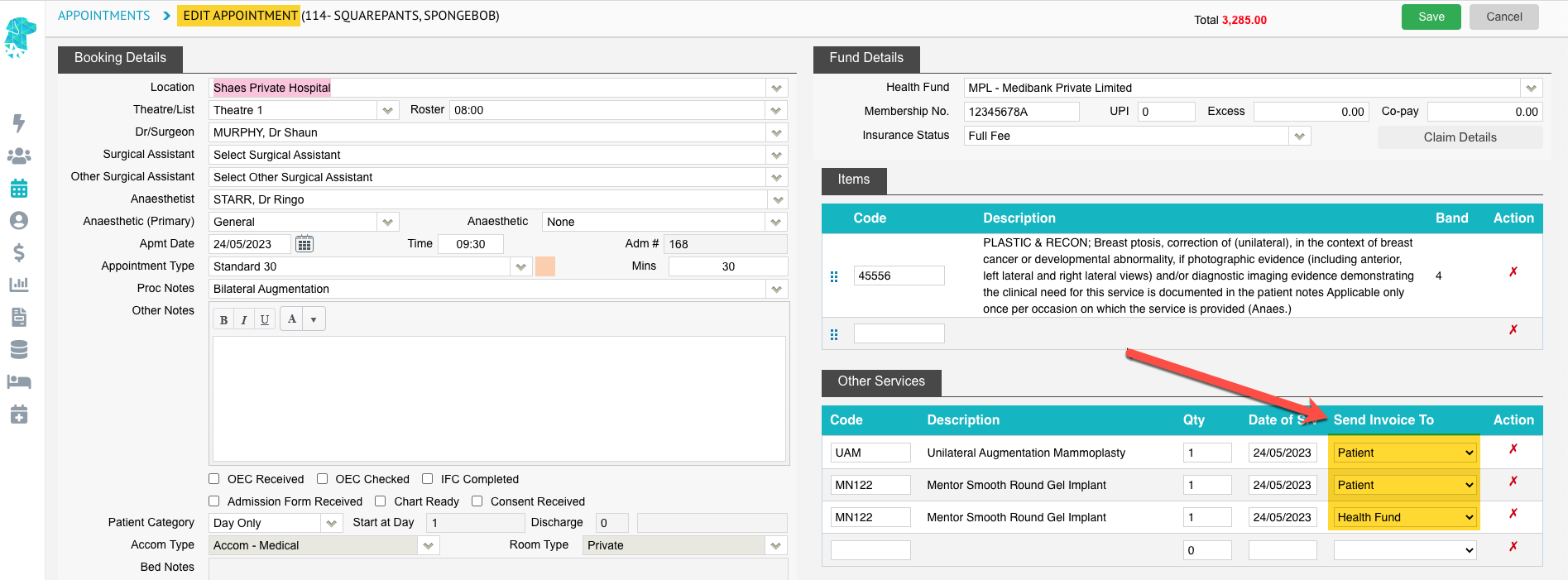
The first step in this process is to ensure the patient is entered with their Health Fund Details for the episode. And then adding the items to the Edit Appointment Screen.
As seen below, FYDO gives the option to Send Invoice To the Health Fund or the Patient. This allows the user to select certain items that will be billed to the patient.
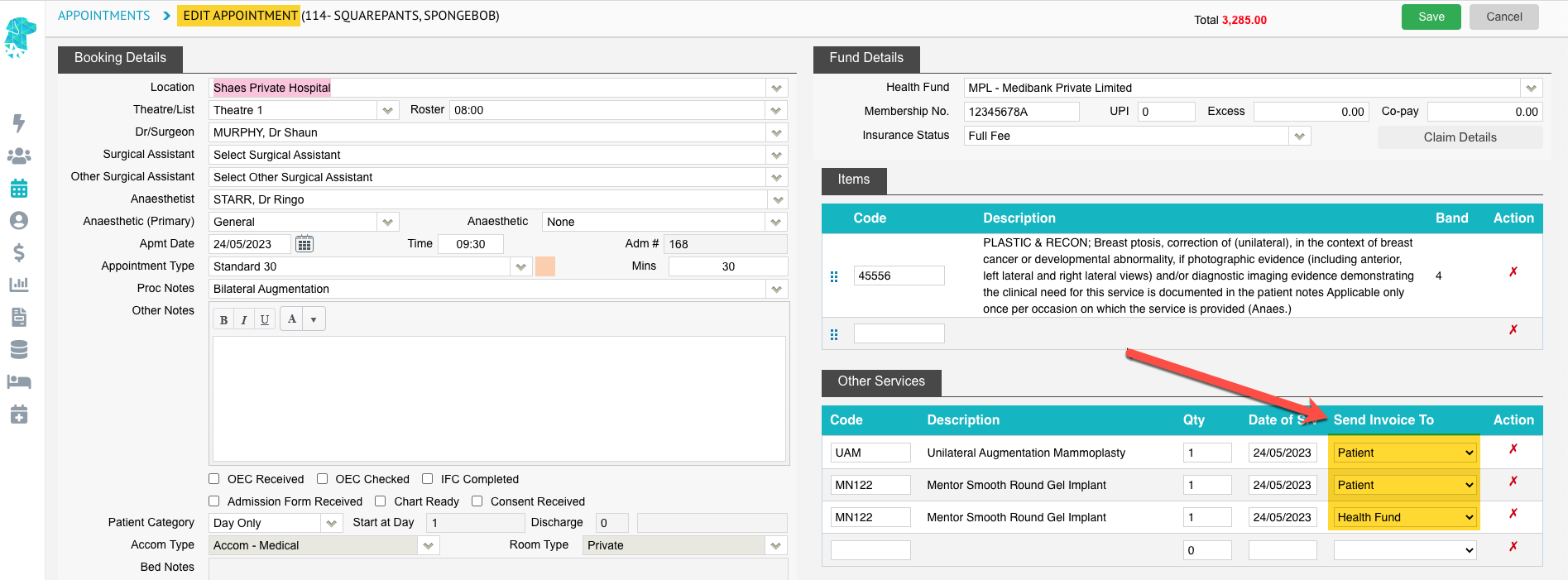
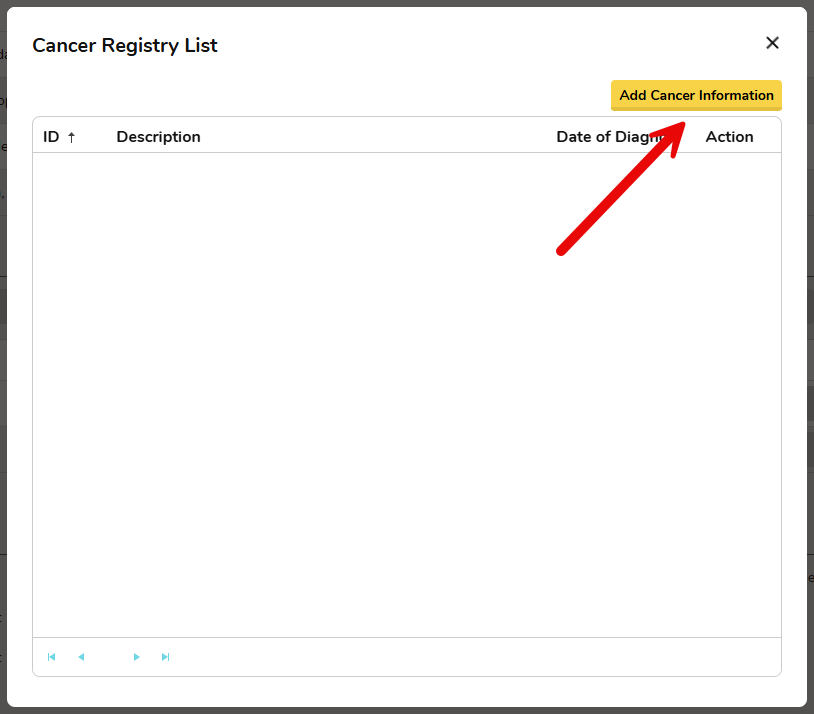
Each facility is able to add their own “codes” to the Other Services list in FYDO. This can be done by following the instructions for Adding Other Services Codes (Hospital) and then adding the corresponding fees by following the instructions for Adding Fees for Other Service Codes (Hospitals)
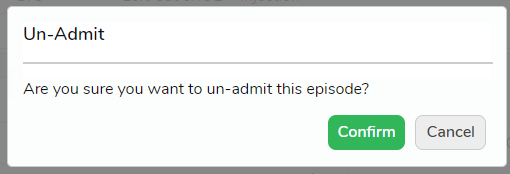
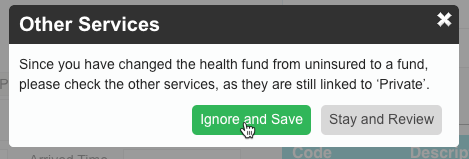
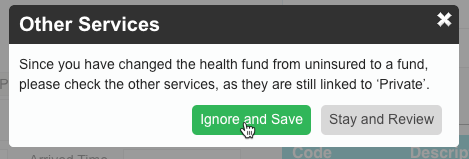
After all required information is entered, the user can click Save. They will then be prompted to review the information, as FYDO wants to be sure that the items are being bill correctly.
Therefore click Ignore and Save.
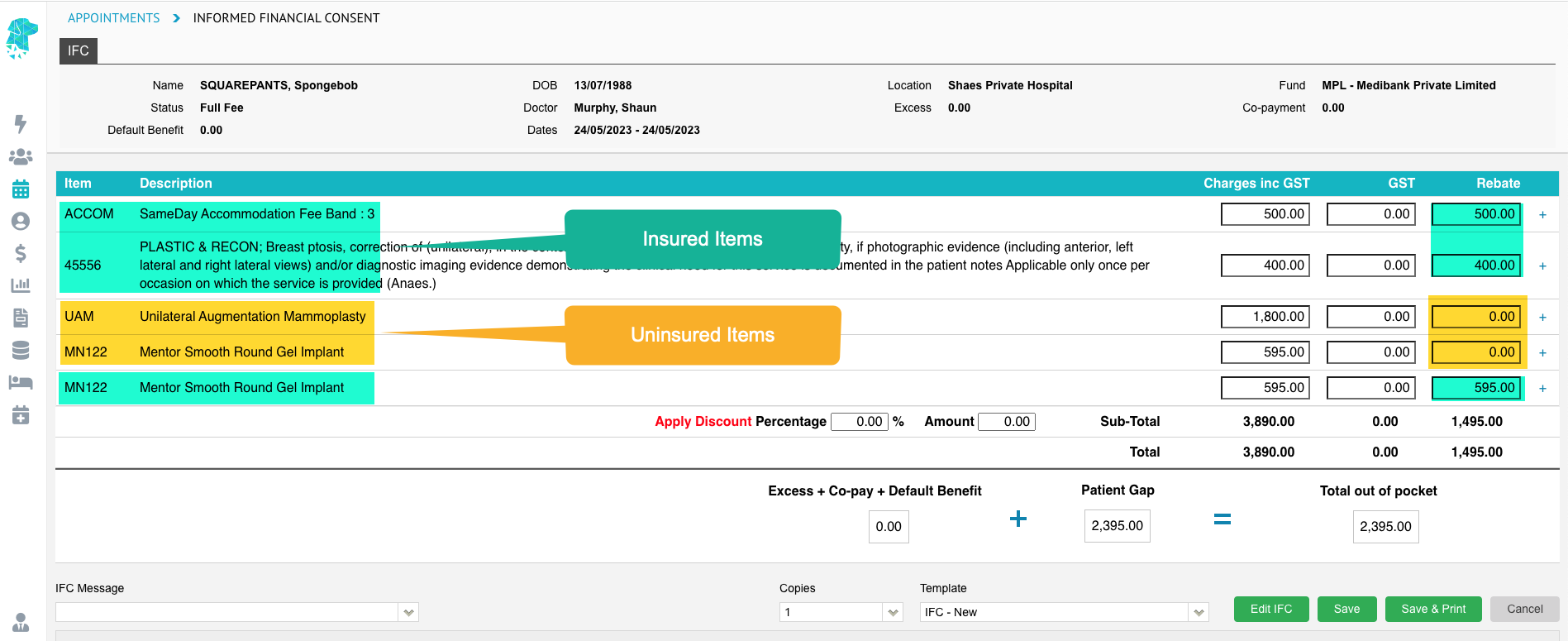
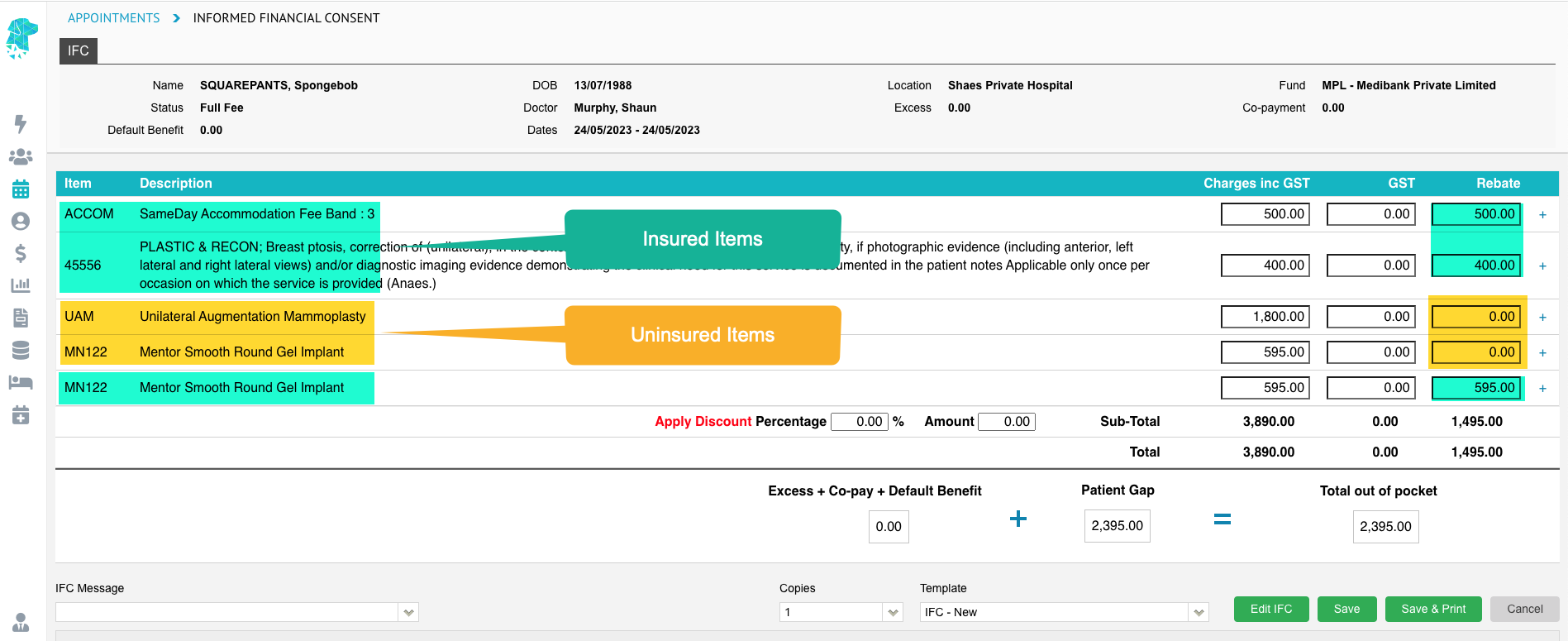
From here, the user is able to proceed to creating the IFC. This is where we will be able to see that the items being billed to the health fund will attract a rebate. And the items being billed to the patient will not attract a rebate.
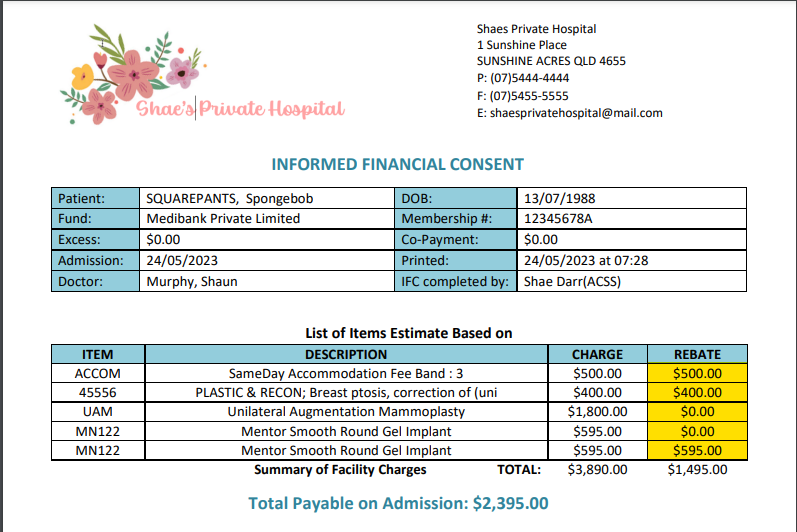
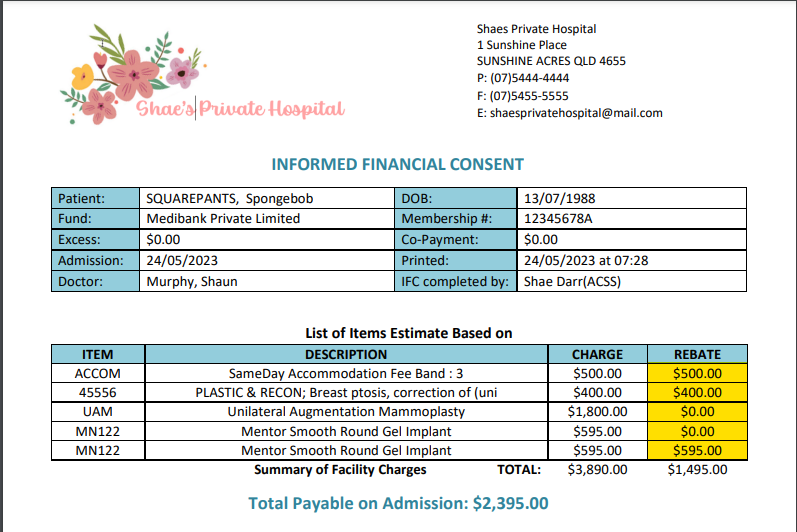
Once the IFC is produced the patient will be able to clearly see which items attract a health fund rebate & which items do not.
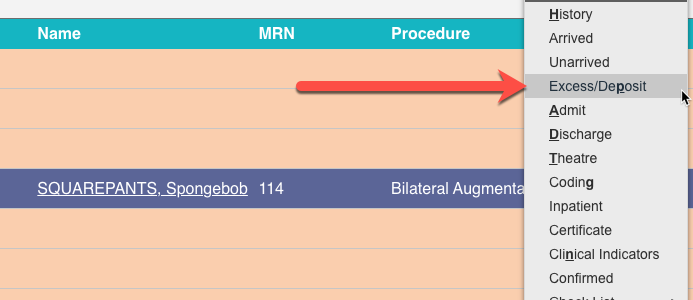
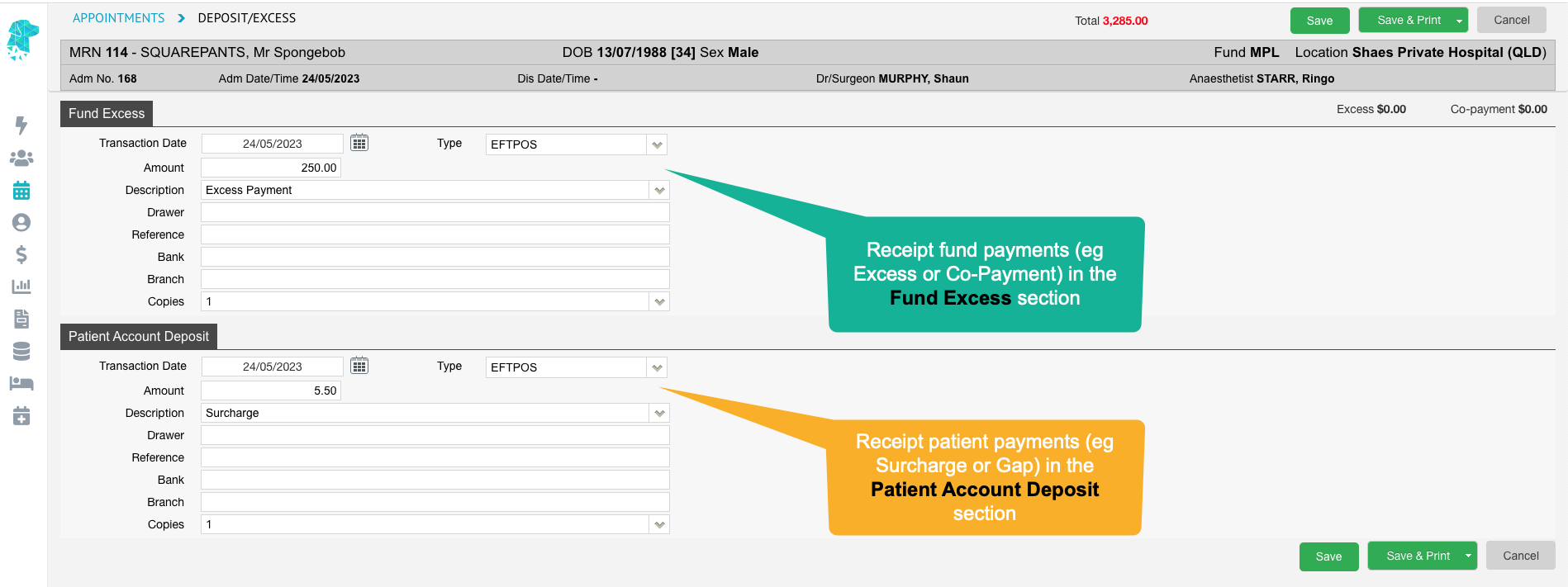
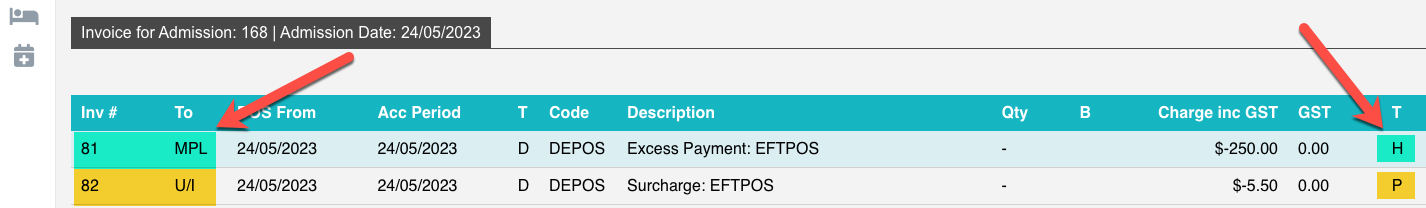
For information in receipting payments for these types of episodes visit these instructions for